CHF and Memory Loss: Understanding Cognitive Decline in Heart Failure Patients

Cognitive decline in heart failure directly impacts your brain’s function, reducing blood flow by up to 30% and disrupting essential memory processes in key areas like the hippocampus.
You’ll notice changes in both immediate and delayed recall abilities, making routine tasks and medication management more challenging.
The condition triggers elevated inflammatory markers (IL-1, IL-6, TNF-α) that disrupt neural communication, while oxidative stress compounds these effects.
Your risk factors include age, heart failure severity, and systemic inflammation, which can accelerate memory loss and executive dysfunction.
Understanding these mechanisms and early warning signs enables more effective management strategies to protect your cognitive health.
Table of Contents
Memory Changes in Heart Disease
The cognitive changes observed in heart disease present a complex interplay between cardiovascular dysfunction and neurological decline.
When you’re living with heart disease, your brain receives less blood flow – sometimes up to 30% less – which directly impacts your memory function.
You’ll typically notice changes in both immediate and delayed recall abilities as the disease progression continues.
You might find yourself struggling with everyday tasks that were once routine.
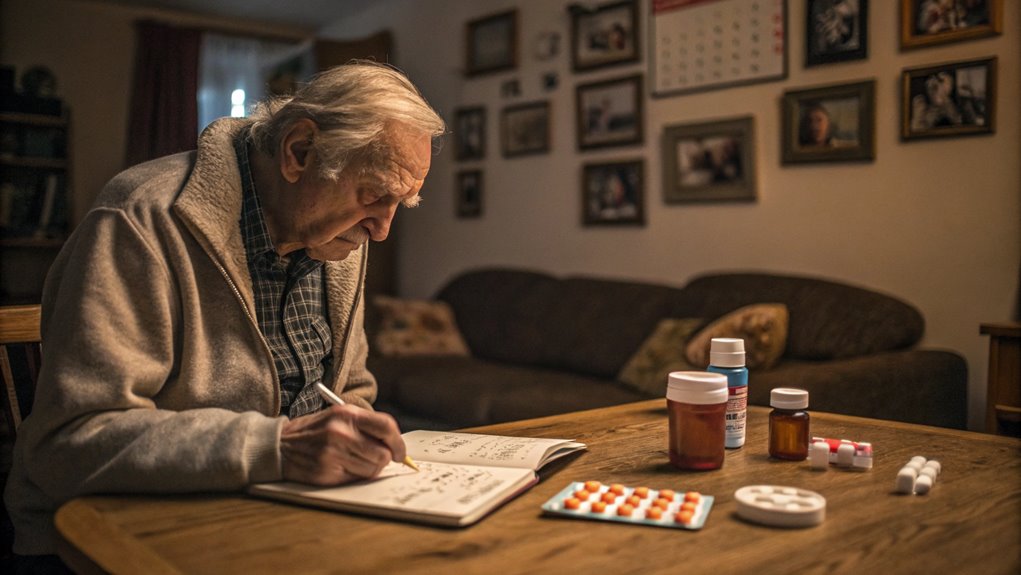
These memory changes often manifest as difficulty remembering medication schedules, forgetting recent conversations, or missing important appointments.
Discover Your Path to a Longer, Healthier Life!
Take our free quiz to see how your lifestyle measures up to the world's longest-living communities and receive expert tips for a healthier, longer life.
Take the QuizThe risk factors that accelerate these memory changes include your age, severity of heart failure, and presence of systemic inflammation.
Your brain’s structure undergoes notable changes, particularly in regions responsible for memory processing.
You’ll experience increased white matter lesions and gray matter loss, especially in areas crucial for memory formation and retention.
These structural changes correlate with the severity of your heart condition – the more advanced your heart failure becomes, the more significant your memory difficulties may be.
Understanding these patterns helps your healthcare team monitor and adjust your treatment plan accordingly.
Brain Health During Heart Failure
During heart failure, your brain’s oxygen supply can decrease by up to 30%, directly impacting memory formation and cognitive processing in critical regions like the hippocampus.
Your blood chemistry undergoes significant alterations, with elevated inflammatory markers (IL-1, IL-6, TNF-α) disrupting neural communication and compromising memory consolidation pathways.
These physiological changes trigger a cascade of neurological effects, including calcium channel dysfunction in neurons and increased oxidative stress, which can accelerate cognitive decline and memory loss.
Oxygen Flow Affects Memory
Oxygen delivery to brain cells plays a pivotal role in memory formation and cognitive processing during heart failure.
When you’re experiencing CHF, your brain receives up to 30% less blood flow, leading to cerebral hypoperfusion effects that directly impact your cognitive abilities.
Your neurons struggle to function properly without adequate oxygen, resulting in memory formation difficulties and slower thought processing.
| Brain Region | Oxygen Reduction | Cognitive Impact |
|---|---|---|
| Hippocampus | 25-30% | Memory loss |
| Frontal Lobe | 20-25% | Executive dysfunction |
| Temporal Lobe | 15-20% | Learning deficits |
| Parietal Lobe | 10-15% | Processing delays |
The oxidative stress impacts from reduced oxygen flow trigger a cascade of cellular damage in your brain.
You’ll notice difficulties with both immediate and delayed recall as neurons struggle to maintain proper function.
Your brain’s white matter becomes increasingly vulnerable to damage, affecting the neural pathways crucial for memory formation.
When oxygen levels consistently remain low, you might experience progressive deterioration in your ability to form new memories and retain information, making it crucial to maintain optimal heart function through prescribed treatments.
Blood Chemistry Changes Effects
Heart failure triggers a cascade of changes in blood chemistry that disrupt the brain’s delicate biochemical balance, leading to cognitive impairments.
These disruptions occur through multiple pathways:
- Altered Blood Composition: The changes interfere with how brain cells communicate and survive.
- Inflammatory Markers: Elevated levels of cytokines like IL-1, IL-6, and TNF-α damage neural tissue and hinder memory formation. If unchecked, they can lead to lasting cellular damage.
- Oxidative Stress: This further compounds the problem by impairing brain cells’ ability to function under these hostile chemical conditions.
- Calcium Channel Dysfunction: The precise electrical signaling required for memory formation and recall is disrupted.
Together, these factors slow cognitive processing and impair memory retention, particularly affecting the ability to learn new information or recall recent events. Long-term memories, however, tend to remain more stable despite these changes.
Early Warning Signs and Symptoms

Recognition of early cognitive decline in CHF patients often begins with subtle yet distinct warning signs.
You’ll notice these changes manifesting through increased difficulty in performing routine tasks, particularly those requiring sustained attention or complex decision-making.
Watch for signs like forgetting medication schedules, missing appointments, or struggling to follow multi-step instructions.
As your healthcare provider monitors your condition, they’ll implement cognitive screening tests to assess changes in your mental function.
You may experience challenges in short-term memory recall, find it harder to concentrate during conversations, or notice a slowdown in processing information.
These symptoms often emerge gradually and may coincide with worsening heart failure symptoms.
Lifespan Comparison Tool
Compare the life expectancy by the U.S. State
Early intervention through lifestyle modifications can help manage these cognitive changes.
You’ll need to pay attention to symptoms like confusion about time or place, difficulty managing finances, or problems following medication instructions.
If you notice these signs, report them immediately to your healthcare team.
The sooner you identify these changes, the more effectively your medical team can adjust your treatment plan and implement strategies to preserve cognitive function.
Treatment Options for Cognitive Decline
Treatment of cognitive decline in CHF patients requires a dual approach: optimizing cardiac medications that support brain function while implementing specialized cognitive therapies.
You’ll find that certain medications, such as ACE inhibitors and beta-blockers, not only improve cardiac output but also help preserve cognitive function through enhanced cerebral perfusion.
When medications aren’t sufficient, device-based interventions like cardiac resynchronization therapy (CRT) can improve both cardiac performance and cognitive outcomes by maintaining consistent blood flow to critical brain regions.
Cognitive Medication Strategies
Medical interventions for cognitive decline in patients with chronic heart failure (CHF) involve a dual approach that integrates heart failure treatments with cognitive-enhancing therapies.
A carefully balanced treatment plan is crucial, as adherence to cardiac medications can become challenging with declining mental function. Key aspects of such interventions include:
- Cognitive-Enhancing Medications:
- Doctors may prescribe acetylcholinesterase inhibitors or memantine for significant memory loss.
- These agents improve neurotransmitter function, enhancing memory and executive function.
- Heart Failure Medication Management:
- Ongoing monitoring ensures heart failure drugs do not negatively impact cognition.
- Special attention is given to beta-blockers that cross the blood-brain barrier, as they can occasionally impair memory.
- Tailored Cognitive Therapies:
- Adjustments to cognitive treatments are made based on heart failure severity and the existing medication regimen.
- Regular Cognitive Assessments:
- Continuous evaluation of cognitive status ensures the treatment strategy remains effective.
Healthcare providers work to optimize brain function while maintaining effective heart failure management, making necessary adjustments to both cardiac and cognitive therapies as the patient’s condition evolves.
Brain-Preserving Device Therapies
Advanced cardiac devices play a crucial role in preserving brain function among CHF patients experiencing cognitive decline.
Through device therapy optimization, you’ll find that cardiac resynchronization therapy (CRT) and left ventricular assist devices (LVADs) can significantly improve cerebral perfusion, potentially slowing cognitive deterioration.
When your healthcare team implements these devices, they’ll carefully monitor your brain’s response to the improved cardiac output.
CRT devices can enhance your heart’s pumping efficiency by up to 25%, leading to better oxygen delivery to your brain tissues.
You’ll often notice improvements in memory and cognitive processing within the first few months of device implementation.
Brain stimulating devices are now emerging as complementary therapies.
These include transcranial magnetic stimulation (TMS) and direct current stimulation devices, which can help maintain neural plasticity and cognitive function.
You’ll typically undergo regular cognitive assessments to measure the effectiveness of these interventions.
Your device settings may require periodic adjustments based on your cognitive performance metrics.
Remember that optimal device programming isn’t just about maintaining cardiac function – it’s equally focused on preserving your brain’s cognitive capabilities through sustained cerebral perfusion.
Support for Caregivers and Patients

Living with CHF-related cognitive decline requires a robust support system that extends beyond clinical care.
You’ll need to implement specific cognitive coping strategies while building reliable emotional support networks to manage daily challenges effectively.
When you’re experiencing memory difficulties, utilize practical tools like smartphone reminders, medication organizers, and written schedules.
You should maintain a detailed symptom diary and establish consistent routines for medication adherence.
These strategies help compensate for cognitive deficits while maintaining independence in disease management.
Your support network should include both professional and personal resources.
Connect with CHF support groups, where you’ll find others facing similar cognitive challenges.
Consider working with occupational therapists who can teach you memory-enhancing techniques specific to CHF management.
Your caregivers should receive training in recognizing cognitive decline symptoms and implementing appropriate interventions.
It’s crucial to communicate openly with your healthcare team about cognitive changes you’re experiencing.
They can adjust treatment plans and provide additional resources as needed.
Remember, early intervention in cognitive decline often leads to better outcomes in both heart failure management and mental function preservation.
Living Well Despite CHF
Three key principles underpin successful daily living with CHF-related cognitive challenges: symptom management optimization, lifestyle modification, and adaptive strategy implementation.
You’ll need to maintain strict adherence to your medication schedule while monitoring daily weight fluctuations and symptoms to prevent exacerbations that could worsen cognitive decline.
Implementing essential lifestyle modifications can significantly impact your cognitive function.
You should prioritize regular, moderate physical activity within your prescribed limits, maintain a heart-healthy diet low in sodium, and ensure adequate sleep quality.
Social engagement plays a crucial role in maintaining cognitive reserves, so you’ll want to participate in community activities and maintain strong social connections when possible.
To combat memory difficulties, you can adopt practical strategies such as using smartphone reminders for medications, keeping a detailed symptom diary, and organizing your living space to minimize cognitive load.
It’s vital to work closely with your healthcare team to adjust these strategies as your needs change.
Remember that successful management requires continuous monitoring and adjustment of both your cardiac and cognitive symptoms, ensuring that one doesn’t adversely affect the other.
Conclusion
Memory challenges may feel like navigating through fog when you’re managing CHF, but you’re equipped with a scientific understanding of the heart-brain connection.
Think of your cognitive health as a parallel pathway to cardiac care – both require vigilant monitoring and intervention.
By implementing evidence-based cognitive preservation strategies alongside your cardiovascular treatment protocol, you’re optimizing both neurological and cardiac outcomes.
Regular assessment of cognitive biomarkers remains crucial for comprehensive disease management.

 972-393-1699
972-393-1699





